Your guide to mRNA vaccines: What is RNA, mRNA and how mRNA vaccines work?

In this article, we will focus on the basics of RNA, mRNA, and how mRNA vaccines work. Let's begin, shall we?
What are RNA and mRNA?
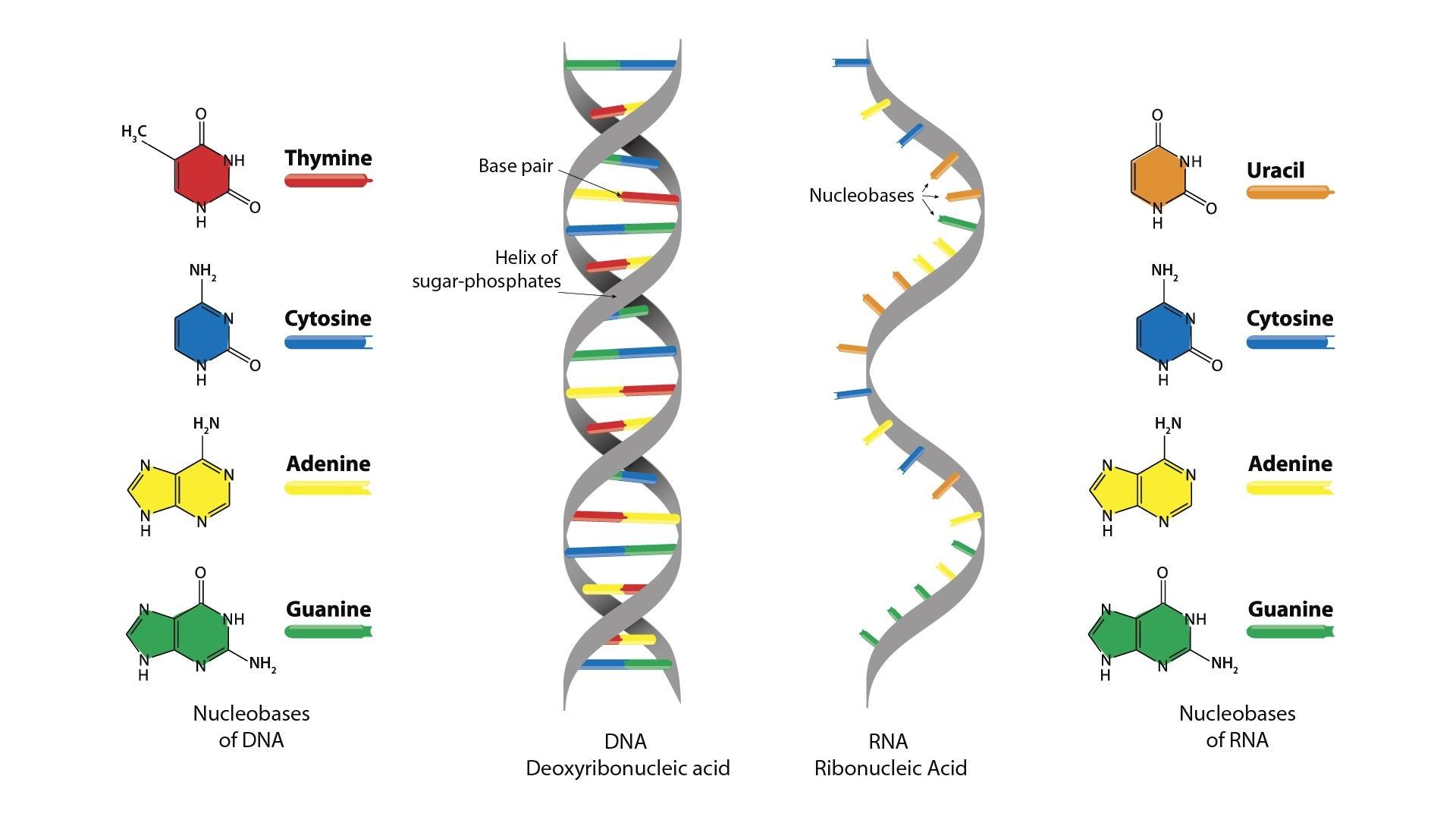
DNA (You can refer to our previous article to understand DNA better) is the genetic material of most organisms on Earth. They are the instruction set to build RNA, or ribonucleic acid (a process called transcription), subsequently protein (by translation), and finally the lifeform. DNA is made up of four types of building blocks (nucleotides): Adenine (A), Thymine (T), Guanine (G), and Cytosine (C). RNA, on the other hand, is made up of A, U (similar to T, replacing T), G, and C.
Codons are nucleotides arranged in groups of three. The grouping in three (eg. AUG, CAG, etc.) can be decoded and translated to chains of amino acids. The arrangement of amino acids in a specific pattern gives polypeptides. In eukaryotes, the RNA molecule undergoes additional processing to form mature messenger RNA (mRNA) before producing a functional end-product - protein.
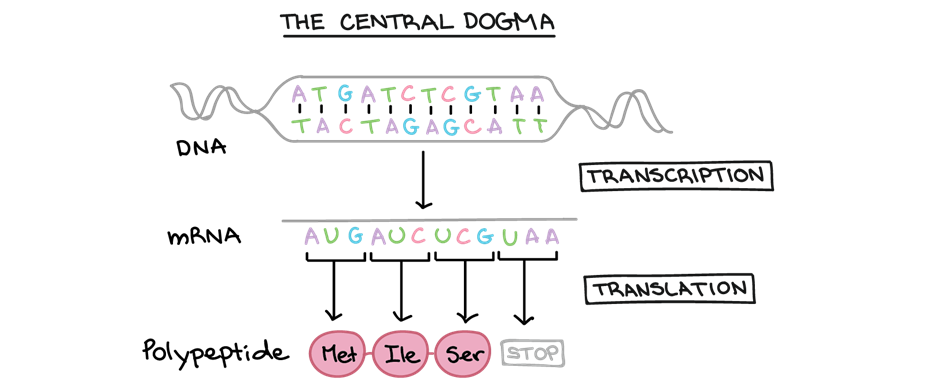
In summary, during the expression of a protein-coding gene, information flows from DNA → RNA → protein. This directional flow of information is known as the central dogma of molecular biology. Non-protein-coding genes are still transcribed to produce an RNA, but this RNA is not translated into a polypeptide (and we will learn more about this in another article). For either type of gene, the process of going from DNA to a functional product is known as gene expression.
What happens during a viral infection?
Have you ever wondered what happens when you catch a cold?
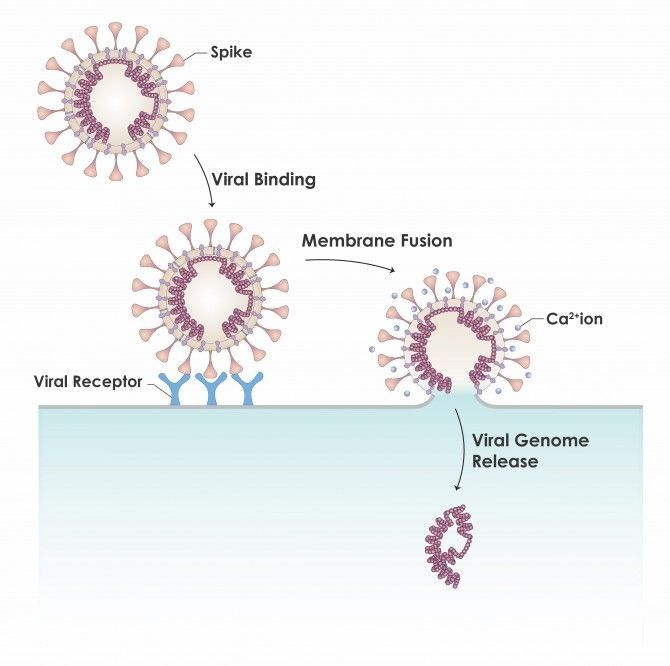
During a viral infection, the virus identifies a suitable host cell and tries to enter. It is impossible to penetrate the cell membrane directly. Lucky for the virus (but unlucky for us), the virus is equipped with a spike protein (they are viral surface proteins) that bind to the host cell surface receptor. During cell entry, the viral membrane fuses with the host cell membrane, and voilà, the virus gets in!
The membrane fusion allows the release of viral genetic material (DNA or RNA) into the host cell. With the viral genetic material inside the host cell, the virus can hijack the host cells to produce more viruses and this ensures the continuity in infecting the surrounding cells.
But, of course, there are policing mechanisms in place to "catch" the infection. Immune cells such as white blood cells recognize virus-associated molecules such as genomic DNA, RNA, or double-stranded RNA (dsRNA) produced by virally infected cells, and initiate effective and appropriate antiviral responses. However, the process takes time and an aggressive virus might have more than enough time to take over the entire body.
So, can we train our bodies to recognize these viruses before they even arrive? This is where vaccines come to the rescue!!
Different types of vaccines
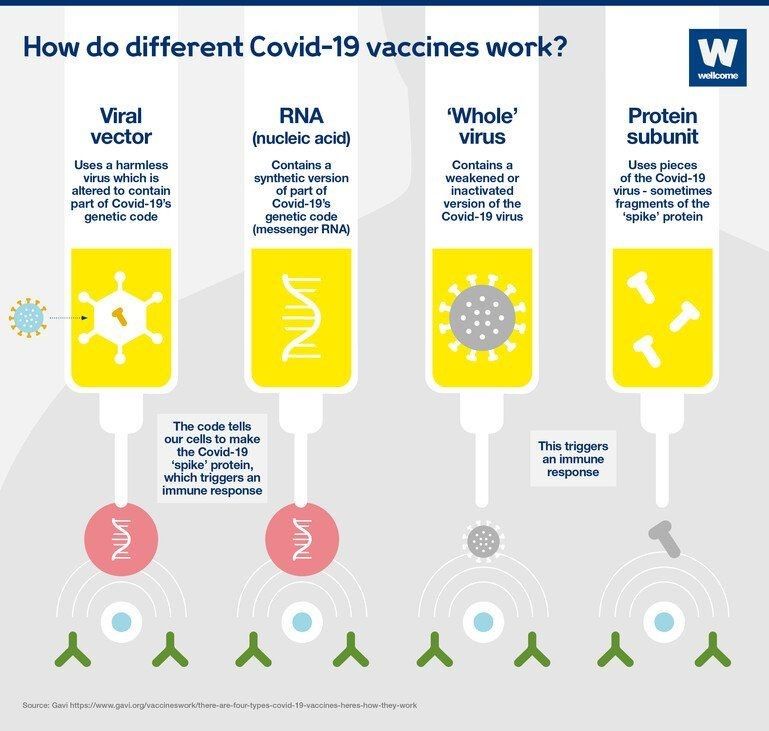
Our immune system is like a dictionary and vaccines are the editors of the dictionary. All vaccines encourage our immune system to produce antibodies, T-cells, or both, so if we encounter the virus in the future, our immune system knows how to defend against it.
Vaccines can evoke an immune response using different technologies. Take the Covid-19 vaccine as an example, there are currently four main approaches:
- viral vector: using harmless, non-pathogenic virus
- RNA: the synthetic version of part of virus genetic code
- whole virus: weakened or inactivated virus
- protein subunit: such as fragments of the spike protein
Read more on the comparison among the different approaches.
How does an mRNA vaccine work? And why mRNA vaccines?
mRNA vaccines consist of mRNA that carries the instructions to make the viral proteins (in most cases spike protein). Upon injection, the mRNA is used as a template to produce the viral spike protein (the viral surface protein). The viral spike protein is non-pathogenic however can trigger an immune response, activating the production of antibodies, T-cells, or both. With repeated dosing of the vaccine, the body then incorporates these cells (B cells - Antibodies, T cells) into its memory repertoire.
When an actual viral infection occurs, the memory T-cells (yes, they have the memory for the bad guy!) will be activated and triggers a series of antiviral responses, thus eliminating the viruses.
Read more about the mRNA vaccine.
Although there are only a handful of Covid-19 mRNA vaccines approved for use (notably Pfizer-BioNTech and Moderna), mRNA vaccines for human use have been studied for infectious agents such as influenza, Zika virus, cytomegalovirus, and Chikungunya virus; and as well for antitumor purposes for over 30 years.
Read more about the tangled history of mRNA vaccines here.
With success in the development of mRNA vaccines against Covid-19 (SARS-Cov2 virus), most notably NIH and Moderna have both recently launched clinical trials of three mRNA HIV vaccines.
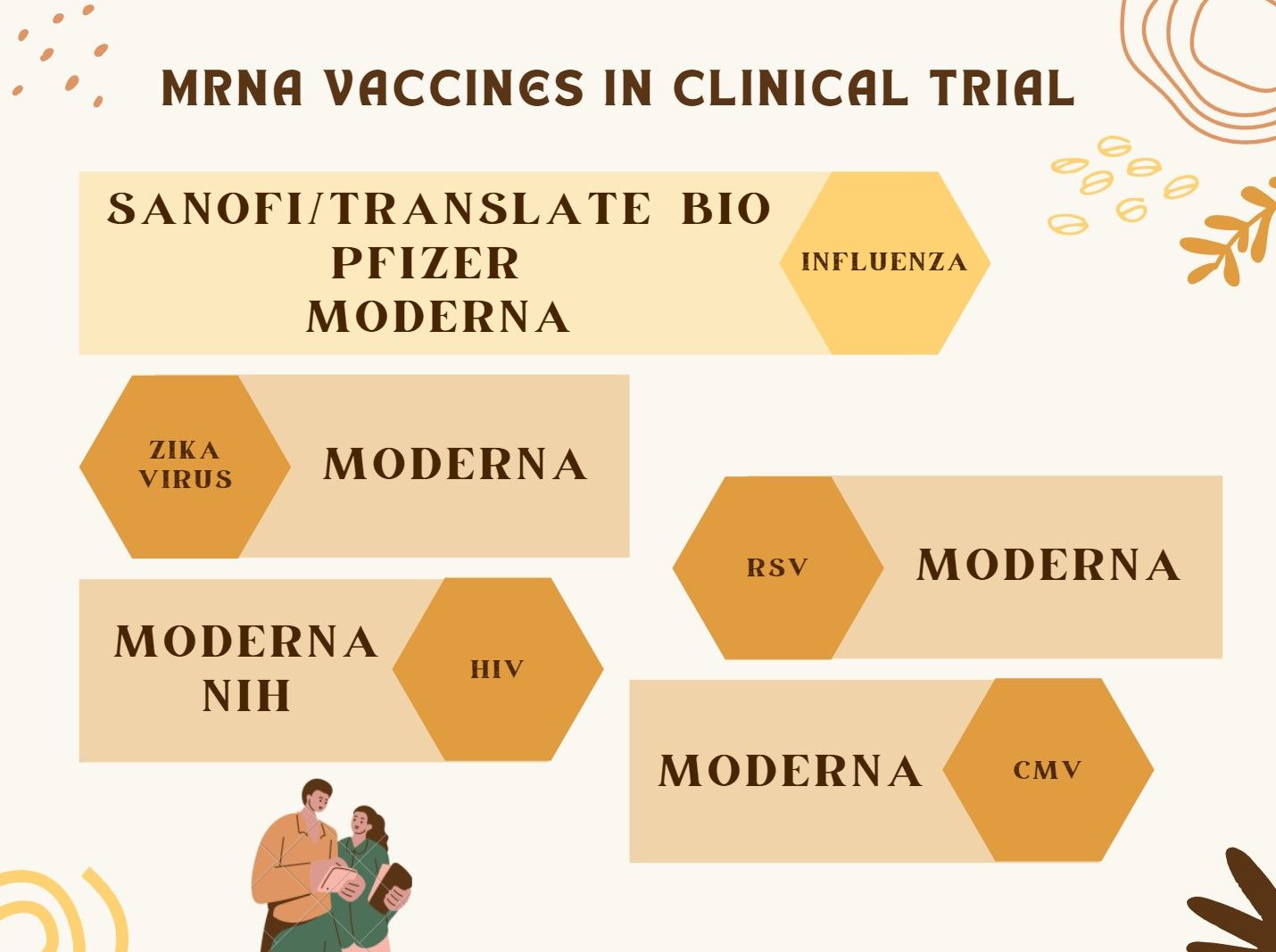
Dozens of clinical trials are also testing mRNA treatment vaccines in people with various types of cancer, including pancreatic cancer, colorectal cancer, and melanoma. These include mRNA vaccines from Moderna, Ludwig Institute for Cancer Research with Boehringer Ingelheim and CureVac, University Medical Center Groningen with BioNTech, and BioNTech with Regeneron Pharmaceuticals.
Read more to find out more about the different mRNA vaccines in clinical trial pipelines.
Closing word
The technology behind mRNA vaccines has been studied for over 30 years. With the success of the Covid-19 vaccines, the world was shown that mRNA technology can be effective as a vaccine modality. And with Pfizer, Moderna, and J&J seeing respiratory syncytial virus (RSV) as the next vaccine target, the excitement for mRNA technology is uncontainable!
Read more here on the excitement for RSV mRNA vaccines.
In the next few articles, we will look at the strengths and weaknesses of mRNA technology as well as other RNA technologies in the market. Stay tuned!
If you liked our article, subscribe to our newsletter to receive our latest articles directly in your inbox. The subscribe button can be found at the corner of the page. We will appreciate your support, or hit the follow button on twitter or Linkedin.
Disclaimer: All opinions shared in this article are the opinions of the authors and do not constitute financial advice or recommendations to buy or sell. Please consult a financial advisor before you make any financial decisions.



Comments ()